
My wish upon on a star would be that ‘undiagnosed brain injury’ and ‘mis-diagnosed brain injury’ no longer happens.
And while I have a star to wish on – can we also have world peace please.
Despite better understanding of brain injury, more sophisticated and efficient diagnostic tools, undiagnosed brain injury continues to happen – and more often than we would wish.
Today Synapse have kindly given permission for me to reprint an article they published in 2011. The magazine “Bridge” is now called Synapse. This links to a previous article on Changed Lives New Journeys Diagnosis and Mis-Diagnosis of Brain Injury The Synapse article reprinted below adds further knowledge about groups at risk of sustaining an undiagnosed brain injury.
I would welcome comments from other countries. While this article speaks of the Australian experience I suspect undiagnosed brain injury within these groups is universal. I also note this article was written in 2011 and I believe not much has changed today.
THE UNDIAGNOSED BRAIN INJURY
Despite increasing awareness of brain injury, there are still many cases that are misdiagnosed or undiagnosed
Although public awareness of Acquired Brain Injury leaves much to be desired, at least within the health professions there is a vast improvement. Some time ago people who reported ongoing cognitive problems after a blow to the head were often ignored as doctors believed there had to be a period of unconsciousness for any lasting injury to occur. Thankfully most health professions are now much better informed, and will often carefully monitor patients until they are fairly sure a brain injury has not occurred.
Misdiagnosis, however, is still a possibility.
WAR VETERANS

Many soldiers have acquired brain injuries as a result of improvised explosive devices (IEDs) in recent wars. Often there is little concern about a brain injury as medics are treating all the other physical injuries that have occurred. There is a growing awareness of IEDS causing a brain injury, but in the past many returning veterans slipped through the net, especially when their symptoms may have been diagnosed as Post-traumatic Stress Disorder.
DOMESTIC VIOLENCE
In Domestic Violence cases ABI (Acquired Brain Injury) assessments may not occur due to the critical nature of the situation. Stress, anxiety and turmoil can continue for months after a blow to the head, so the symptoms of a brain injury can often be hidden.
DUAL DIAGNOSIS
Dual Diagnosis is a common occurrence in people with ABI. Put simply, this is when two disorders are affecting an individual at the same time. This could be someone presenting with a brain injury along with depression, anxiety, Post-traumatic Stress Disorder, or a dependency on alcohol or other drugs. As with war veterans, treatment in crisis situations may mean that a health professional may not even be looking for the underlying symptoms of a brain injury. Even when they are, diagnosis can be difficult as the symptoms of a brain injury can often mimic symptoms of Mental Health issues resulting in an incorrect or incomplete diagnosis.
Click the image on the left to obtain a free PDF copy of the book Mental Health and ABI.
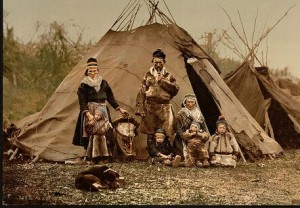
INDIGENOUS COMMUNITIES

Recent research suggests that brain injuries may be far more prevalent in some Aboriginal and Torres Strait Islander communities than realised. The major causes are domestic violence, dependency on alcohol and other drugs, and foetal alcohol syndrome. Again, misdiagnosis may occur because intervention is focussed on substance use, or treating physical injuries. Complicating this is the appalling lack of services to many Aboriginal and Torres Strait Islander communities, meaning that services either don’t exist, or are overstretched, and so many brain injuries go undiagnosed. The statistics for Aboriginal and Torres Strait Islanders are clear:
• Brain injury from assault was 21 times higher than in non Aboriginal and Torres Strait Islanders.(1)
• Females were 69 times more likely to be injured than in non Aboriginal and Torres Strait Islanders(1)
• In 2002, one in six Aboriginal and Torres Strait Islanders aged 15 years or over reported risky/high risk alcohol consumption in the last 12 months.(2)
LACK OF HEALTHCARE SERVICES
In the developing world, there are many regions that either have no healthcare services, or families in poverty are unable to afford services. There are no statistics available in these situations, but one can only wonder at the numbers of people worldwide who are struggling with the symptoms of a brain injury, yet not aware that they have one. This is particularly salient when taking in to account the recent disasters occurring around the world.
FOOTNOTES
1 “Hospitalisation for head injury due to assault among Indigenous and non-Indigenous Australians”, Lisa M Jamieson, James E. Harrison and Jesia G. Berry, Medical Journal of Australia, 2008; 188 (10): 576-579.
2 The Health and Welfare of Australia’s Aboriginal and Torres Strait Islander Peoples, Australian Bureau of Statistics, 2005.
If you would like to read more articles from this magazine or others published by Synapse there is a range of Fact Sheets and Reading HERE
There are many stories illustrating the impact of undiagnosed brain injury here is a link to one article ” Undiagnosed Brain Injury is Behind A Soldiers Suicidal Thoughts” that I read recently.


Pingback: RePost: Rant for Remembrance - Soldiers With Brain Injury - Changed Lives New Journeys